Can Microbiomes Treat Gout One Day?
Ever since Barry Davis contacted me and agreed to write the guest post on his personal bout with gout, and how he thinks that parasite bacteria in our gut may be the root cause of gout, I have been doing more research on the subject and my findings will surprise you. For those who haven’t read Barry’s post, I recommend that you do before continuing reading this post.
Although my research didn’t find anything relating gout with a leaky gut, there is a lot of evidence relating leaky gut with autoimmune diseases (gout is an autoimmune disease) like rheumatoid arthritis and psoriasis, which are closely related to gout.
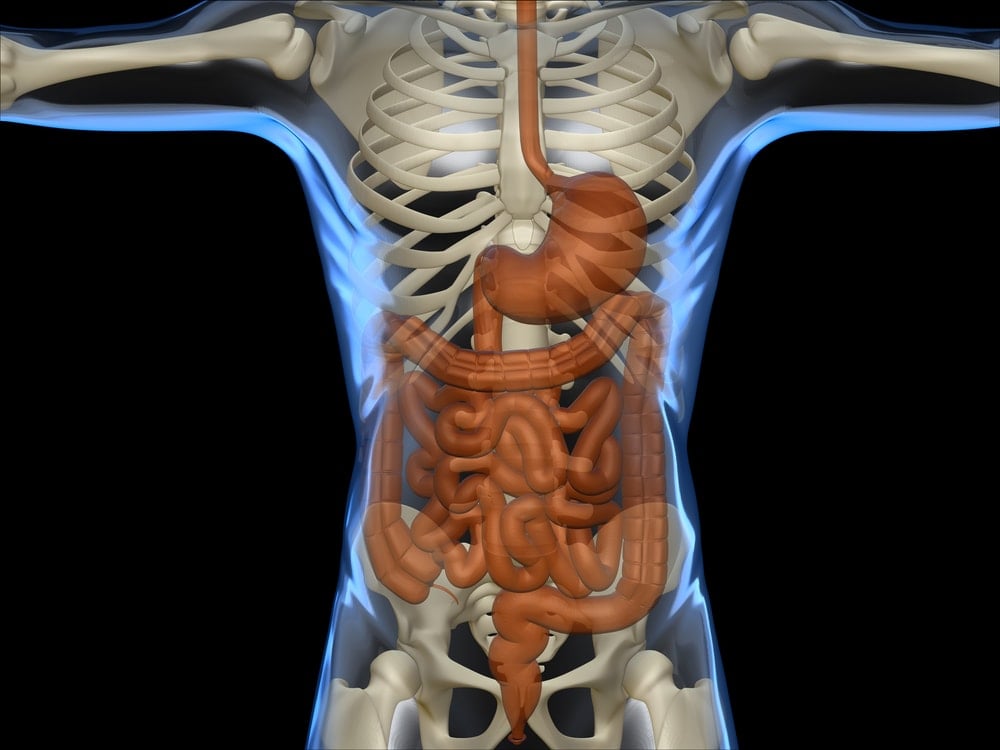
So what is a leaky gut? I found the best definition in Dr.Weil’s site:
“Leaky gut syndrome is not generally recognized by conventional physicians, but evidence is accumulating that it is a real condition that affects the lining of the intestines. The theory is that leaky gut syndrome (also called increased intestinal permeability), is the result of damage to the intestinal lining, making it less able to protect the internal environment as well as to filter needed nutrients and other biological substances.
As a consequence, some bacteria and their toxins, incompletely digested proteins and fats, and waste not normally absorbed may “leak” out of the intestines into the blood stream. This triggers an autoimmune reaction, which can lead to gastrointestinal problems such as abdominal bloating, excessive gas and cramps, fatigue, food sensitivities, joint pain, skin rashes, and autoimmunity. The cause of this syndrome may be chronic inflammation, food sensitivity, damage from taking large amounts of nonsteroidal anti-inflammatory drugs (NSAIDS), cytotoxic drugs and radiation or certain antibiotics, excessive alcohol consumption, or compromised immunity.”
In a 2021 study published in NPJ Biofilms and Microbiomes found that compared to healthy individuals, patients with gout were found to have a significantly unique gut microbiota associated with dysregulated host urate degradation and systemic inflammation.
The researchers concluded, “Our results showed a dysbiosis of gut microbiome in gout that was associated with increased serum uric acid and systemic inflammation and may be partially restored by uric-acid-lowering and anti-inflammatory drug interventions over time.”
Let’s Examine the Evidence
So let’s continue with my findings. Firstly, an interesting article about a woman and her bout with psoriasis can be read at psoriasis.org. She goes on to say how she developed the disease at the age of 14 and how a friend recommended that she try probiotics. After a few days she credited the probiotics for clearing her psoriasis. By taking probiotics, you basically introduce new bacteria into the gut. Others eat certain foods to modify their microbiome. Think Greek yogurt!
Did you know that our bodies have about 100 trillion microbial cells? Microbes actually tell our immune system what to do. Researchers know that our immune system targets microbes and that’s how it defends us from harmful pathogens.
“Microbes have figured out our immune system in ways that we, as scientists, still don’t fully understand,” said Sarkis Mazmanian, a microbiologist at the California Institute of Technology.
“We rely on our immune system to distinguish between microbial invaders that might make us sick and the harmless bacteria that are always inside us,” said Mazmanian. Based on this distinction, the immune system decides when and when not to attack. But the immune system doesn’t make this decision by itself.
“Part of the decision-making process is actually controlled by specific gut microbes,” said Mazmanian.
Basically, these bugs call the shots! This means that microbes contribute to our body’s decision of whether to launch an immune attack like rheumatoid arthritis, psoriasis and possibly gout too! It’s not out of the question.
There is an interesting study that appeared in June 2010 issue of Immunity conducted with mice. Scientists had germ-free mice engineered to have some mild arthritis ingest a certain kind of bacteria after which they developed a more severe form of arthritis. Scientists learned two important things with this study. One that throwing bacteria off balance can lead to inflammatory disease and that this disease doesn’t necessarily have to occur where the bacteria are located. In conclusion, bacteria in the gut can trigger inflammation outside the gut.
“Scientists can’t create bug-free people to see if they develop autoimmune disorders. But they can look at the bugs that people with autoimmune disorders have to see whether any particular microbes might correlate to disease development,” said Melissa Leavitt associate director of scientific communication for the National Psoriasis Foundation.
She goes on to say, “Jose Scher, a rheumatologist at New York University, is exploring whether the gut microbiome of people with psoriatic arthritis differs from that of healthy people. His preliminary findings suggest that people with psoriatic arthritis may have less bacterial diversity, which means they have depleted supplies of some kinds of bacteria.” Could this be true also for gout? I wonder.
Jose Scher goes on to say how people with rheumatoid arthritis were much more likely to have a bug called Prevotella copri in their intestines than people that did not have the disease. Scher also found that patients with psoriatic arthritis, another kind of autoimmune joint disease, had significantly lower levels of other types of intestinal bacteria. Scher thinks that eventually, it will be possible to treat arthritis by adjusting the microbiome!
According to Martin Blaser, the director of the Human Microbiome Program, “Probiotic treatments would be designed to have the opposite effect — instead of killing the bad bugs, they would promote the good ones, the ones that reduce inflammation involved in psoriatic disease. But these, too, would be different from what’s on the market now.”
“Scientists may eventually develop an entirely new class of probiotics,” Blaser said, that would be highly targeted to address psoriasis.
Diet is Key Folks! Forget What The Naysayers think!
Going back to Jose Scher, I had to add this in, cause I like it when doctors are aligned with my diet philosophy. Read the following from theAtlantic:
“Scher puts more faith in modifying the microbiome through diet. He notes that some patients with rheumatoid arthritis have benefitted from cutting out meat, or adopting a Mediterranean diet (high in fish, olive oil, and vegetables, and low in meat and saturated fat), though scientists don’t know exactly why this helps.
In a separate study, Finnish researchers found that a vegan diet changed the gut microbiome, and that this change was linked to an improvement in arthritis symptoms.”
Leaky gut causes many disorders including:
- Rheumatoid arthritis
- Psoriasis and Eczema
- Celiac disease
- Allergies and Asthma
- Inflammatory Bowel disease
- Multiple Sclerosis
- Food allergies
- Liver and gallbladder disease
- Thyroid
- All I found for gout was a 2005 study about the importance of the intestinal tract in the elimination of uric acid but it seems more research needs to be done in regards to gout and leaky gut.
There is a new study though from the University of Otago that a gene called PDZK1 which controls the amount of uric acid gets excreted from the kidney and gut, is not sufficiently produced in some gout sufferers. By understating the genetic variations amongst different gout patients, we can treat everyone differently through precision medicine. This is the future of medicine! Exciting!
In a study published in Nutrition, Metabolism and Cardiovascular Diseases discovered a causal relationship between gut microbiota and risk for hyperuricemia. It investigated the link between specific bacterial genera and uric acid levels. The study found that Escherichia-Shigella was associated with an increased risk of hyperuricemia, while Lachnospiraceae and Family XIII AD3011 were linked to a reduced risk. The authors suggest that these findings could inform the development of new therapeutic approaches for gout and hyperuricemia, such as probiotics or fecal microbiota transplantation. However, the study does have limitations, including the analysis at genus level only and the predominantly European study population.
In conclusion, this is an exciting new area for medicine to focus on and many researchers believe that in 10 to 15 years that the microbiome will be a key therapeutic option for some of these diseases. For those that want to dig in further, I have also linked to this interesting article from Nature.com.